Mental Health and the Climate Crisis– Daniel Rosenbaum, Eric Brown, Siqi Xue
Life, Death, and Urban Health under Climate Change– Laura Rosella, Inori Roy, Kim Perrotta
Environmental Co-Benefits of Reducing Low-Value Care – Thomas Bodley, Brenda Change, Anita Rao
Quality Improvement to Reduce the Environmental Impact of Health Care – Thomas Bodley, Christine McDonald, Melissa Ho, Sarah Bunston
Hot Topics in Sustainable Prescribing Practices
Research for Climate, Health & Sustainable Care – Jimin Lee, Jacques du Plessis, Jeffrey D’Souza
Health Professions Education – Amna Zafar & Jefin Mathews, Marlee Vinegar, Laura Feldman & Katherin Yu, Karen Cameron & Maria Mylopoulos
Sustainable and Climate Conscious Clinical Care – Grace Kuang, Charmi Shah, Pierette Price Arsenault
Governance & System Change for Sustainable Health Systems – Melanie Seabrook & Sara Allin, Carlene van der Helden, Camila Heredia, Brittany Barber
| Author(s) | Title | Abstract |
|---|---|---|
| Parker et al. | Mapping the Environmental Co-Benefits of Reducing Low-Value Care: A Scoping Review and Bibliometric Analysis | Reducing low-value care (LVC) and improving healthcare’s climate readiness are critical factors for improving the sustainability of health systems. Care practices that have been deemed low or no-value generate carbon emissions, waste and pollution without improving patient or population health. There is nascent, but growing, research and evaluation to inform practice change focused on the environmental co-benefits of reducing LVC. The objective of this study was to develop foundational knowledge of this field through a scoping review and bibliometric analysis. We searched four databases, Medline, Embase, Scopus and CINAHL, and followed established scoping review and bibliometric analysis methodology to collect and analyze the data. A total of 145 publications met the inclusion criteria and were published between 2013 and July 2023, with over 80% published since 2020. Empirical studies comprised 21%, while commentary or opinions comprised 51% of publications. The majority focused on healthcare generally (27%), laboratory testing (14%), and medications (14%). Empirical publications covered a broad range of environmental issues with general and practice-specific ‘Greenhouse gas (GHG) emissions’, ‘waste management’ and ‘resource use’ as most common topics. Reducing practice-specific ‘GHG emissions’ was the most commonly reported environmental outcome. The bibliometric analysis revealed nine international collaboration networks producing work on eight key healthcare areas. The nineteen ‘top’ authors were primarily from the US, Australia and Canada. |
| Zgardau et al. | Carbon Footprint Reduction associated with Multidisciplinary Pediatric Airway Clinics | Objective: Multidisciplinary clinics may reduce carbon emissions by combining multiple appointments into one. This is the first program evaluation study to quantify the carbon footprint associated with multidisciplinary pediatric airway clinics. Methods: Pediatric airway multidisciplinary clinics allow patients to see otolaryngology and respirology in one appointment. The carbon and financial savings (Canadian Dollars) of all patients attending the multidisciplinary clinic at the Children’s Hospital at London Health Sciences Center, London, Canada, from January 1, 2018-December 31, 2022, were calculated. Patient postal codes and institutional parking rates were inputted into the CASCADES carbon accounting tool. Total distance was divided into unsustainable (vehicles) and sustainable (transit, cycling) transportation to calculate carbon emissions. Travel costs included cost/kilometer for vehicles and costs/ride for transit. Results: 560 multidisciplinary clinic appointments for 300 patients saved 77,785 KM. Total carbon emissions saved from travel averted was 16.21 tonnes. The total carbon emissions saved, minus public transit, was 15.60 tonnes. Using Natural Resources Canada Greenhouse Gas Equivalencies Calculator, 16.21 tonnes are approximately equivalent to 5 passenger vehicles, 6,906L of gasoline, 3.8 homes’ energy and 10.8 homes’ electricity use for one year, 36.6 barrels of oil consumed, and 675 propane cylinders. Travel costs of $28,891.83 (no parking), $30,519.40 ($4 minimum parking fee), or $33,774.55 ($12 maximum parking fee) was saved. Discussion: Healthcare is a significant contributor to the climate crisis. Multidisciplinary clinics effectively reduced carbon emissions and offered patients financial savings. Implications for Practice: Similar multidisciplinary clinic models can be adapted across institutions to help mitigate climate change. |
| Joseph et al. | An Investigation of the University of Toronto’s Nursing Program’s Integration of Planetary Health Using the Student-led PHRC Tool | Planetary health is the understanding that human health and the environment are interconnected, emphasizing the need for stewardship. The planetary health report card (PHRC) is a student-led tool used globally to evaluate and enhance healthcare schools’ focus on planetary health and sustainability in healthcare advocacy through a letter-graded report card. To explore planetary health strengths and opportunities for growth within the University of Toronto (UofT) nursing program, to implement and optimize planetary health in the curriculum and program, and to advance the global planetary health movement for a healthier and more equitable world. There are five categories of the 2023 PHRC which include: the planetary health curriculum, interdisciplinary research, community outreach and advocacy, support for student-led planetary health initiatives, and campus sustainability. Five teams of nursing undergraduate students used school websites, the 2023-2024 curriculum, student initiatives, and communicated with faculty members to complete the tool. The scores from each category were then associated with a letter grade rubric. Overall, the institutional grade for the Lawrence Bloomberg Faculty of Nursing at UofT was a C. Based on the results of the report card, three initiatives were proposed. First, the initiation of a sustainability committee, to outline specific sustainability guidelines inclusive of the sim lab. Secondly, the incorporation of more planetary health topics throughout the entire curriculum. Finally, increasing the awareness and accessibility of sustainability topics by showcasing student resources on campus, through the website and email communication. These proposed initiatives lay the foundation for building, improving and tracking the progress of planetary health and sustainability in our nursing program. |
| Munir et al. | The Effects of Exposure to Air Pollution on Obesity and Obesity-related anthropometric measurements: A Systematic Review and Meta-analysis | Background and objectives: The association of air pollution with body fat distribution has been studied observationally, but results have been inconclusive. The present study sought to determine the impact of ambient air pollutants on obesity and the most frequently used anthropometric measurements related to obesity. Approach: We searched the following databases: OVID Medline, Embase, PubMed, Web of Science, LILACS and grey literature from inception until October 30, 2023, and updated on January 23, 2024, using a comprehensive search strategy. Two independent reviewers assessed the eligibility of articles and extracted the data. A meta-analysis was conducted for all outcomes with two or more studies. Results: We analyzed 35 studies, of which 22 were from a middle-income country (China), and 13 from high-income countries. The meta-analysis revealed that increase in PM2.5 (per 10 μg/m3) and NO2 (per 10-ppb) were associated with an increase in Body mass index (BMI) of 0.77 (95% CI: 0.56, 0.98) and 1.40 (95% CI: 0.84, 1.95) kg/m2 respectively, with obesity odds increasing by 13% [Odds ratio (OR), 1.13 (95% CI: 1.08,1.18)] and 39% [OR, 1.39 (95% CI: 1.23, 1.57)] respectively and the obesity risk increasing by 8% [HR, 1.08 (95% CI: 1.06 to 1.11)] and 7% [Hazard Ratio (HR), 1.07 (95% CI: 0.95 to 1.22)] respectively. Moreover, PM2.5 (per 10 μg/m3), and NO2 (per 10 ppb) were associated with 1.17 (95% CI: 0.58, 1.75) and 18.51 (95% CI: 5.31, 31.71) cm increase in waist circumference (WC) and increased odds of abdominal obesity by 17% [OR, 1.17 (95% CI: 1.11 to 1.23)] and 64% [OR, 1.64 (95% CI: 1.28 to 2.10)] respectively. |
| Sánchez-Pimienta | Re-imagining Planetary Health Categories | Background and objectives: Planetary health appears like a promising framework to make sense of the health of humans and more-than-humans in the Anthropocene/Capitalocene/Chthulucene. Indeed, this framework invites researchers and practitioners to see “humans as part of nature” and include Indigenous Knowledges. However, the very notions of “Human” and “Nature” are cultural constructions of Western philosophy. My objective is to explore whether these categories are appropriate for understanding planetary health across the globe. Approach: In this poster, I share two stories illustrating the limitations of the Human and Nature categories to understand the efforts of two Mexican communities striving for environmental health in a region polluted by over 700 industrial enterprises. Outcomes: The story about Nature conveys two ways of determining water quality and pollution, one based on the threshold theory of pollution and the other based on the presence or absence of native animals in this watershed. The story about the Human category discusses a case of reclamation of Indigenous identities in Juanacatlán and reflects on the potential perils of studying this case as part of my dissertation research. Impact: Taken together, the first story invites readers to consider alternative relationships between scientific and community knowledge. Additionally, the second story highlights the importance of reverting the gaze to the researchers’ positionality as a more ethical approach than studying the “Other.” |
| Cuppage | Digital Health and Sustainability: Opportunities and Challenges | Background and Objectives: The World Health Organization has deemed climate change the “biggest health threat of the 21st century.” Climate change will have devastating impacts on the health of individuals, most felt by equity-deserving groups, which are already being experienced in Toronto. The health care sector in Canada accounts for approximately 4.6% of the country’s total emissions, contributing to climate harms to patients. Digital health technologies have the potential to catalyze transformative change in the health system, and the goal of this Executive Master of Health Informatics Project was to explore the opportunities for digital health to advance climate action and climate resiliency in health care, as well as explore the potential climate harms related to digital health technologies. Approach: A literature search was conducted on digital health and environmental sustainability. Meetings were held with a variety of interest holders including hospital facilities and environmental services leaders, digital health leaders, clinical leaders, and sustainability leaders. Outcomes: Several frameworks exploring the intersection of digital health and sustainability were identified. Findings were synthesized into five top areas of focus for leveraging digital health to improve environmental sustainability of health care, and four areas of challenges related to the negative environmental impacts of digital health. Interest holder meetings revealed that within a hospital, climate-related data spans all areas of the organization, and that there are many potential options for reporting, including organizational scorecards, quality improvement plans, and benchmarking tools. Results/impact: There are many ways that digital health may be harnessed to improve the environmental sustainability of the health care system. These potential benefits need to be weighed against the potential climate related risks posed by the expansion of digital health technologies. |
| Riad et al. | Effects of Climate Change on Patients with Chronic Conditions and their Healthcare Providers– Knowledge, Perceptions, and Attitudes: a Scoping Review | Background: Persons living with chronic conditions face heightened risk to their health from climate change impacts. Individuals, health care providers (HCPs) and decision-makers/policymakers need to be aware of these impacts to ensure the best quality of care. Our objective is to synthesize an understanding of the knowledge, perceptions, and attitudes about climate change impacts on health outcomes of Canadian HCPs and patients living with chronic conditions. Methods: A scoping review search was carried out to identify published studies in any language between January 2010 and June 2024. Electronic databases MEDLINE, EMBASE, and PsycINFO, were searched. Eligible studies included studies that reported any of the outcomes related to the knowledge, perceptions and/ or attitudes of any Canadian HCPs and/or any Canadian patients living with a chronic condition. The study had to link the knowledge, perceptions and/ or attitudes to climate change. Two reviewers were independently responsible for data screening and extraction using Covidence and Microsoft Excel, respectively. Results: 5948 citations were screened and only 3 studies met the inclusion criteria. Two studies were international cross-sectional studies and included Canadians, while one was conducted in Canada only. A study examined the knowledge and attitudes of HCPs regarding the link between climate change and kidney health. Reported outcomes varied widely in terms of perceived risk from climate change, the degree of personal control over these risks, and acceptable levels of risk to HCPs. While concern about climate change’s impact on patient health showed mixed results across studies, there was a consistent and high level of understanding that climate change negatively affects patients with chronic conditions. Knowledge of climate change among HCPs was also mixed, with two out of three studies reporting that less than half of participants felt adequately informed to support patients. None of the included studies focused on the knowledge, perceptions, and attitudes of patients living with a chronic condition, although one study contrasted HCPs to the general Canadian public. |
| Amoah et al. | Compounding effects in climate change and health equity: Inclusivity in discourse and response generation | Background and objectives: Climate change exacerbates health and social inequalities, with poverty both increasing exposure to environmental risks and resulting from such exposure. The compounding risks of climate change intensify these inequalities and require consideration for mitigation and adaptation efforts to be effective. An inclusive approach in discourse and response generation is essential, especially considering the specific risks faced in Canada. The unique challenges to health equity within the Canadian context need to be identified and articulated. This research aimed to reveal the specific and crosscutting implications of climate change on women, homeless populations and immigrants in Canada, and to provide tailored recommendations for adaptation and mitigation strategies that address the needs of these populations. Approach: The research drew on results of an analysis of media discourses on climate change, poverty and women’s health issues, a commentary piece on the inclusion of migrants in national adaptation strategies, and a rapid review of health impacts of extreme heat on homeless populations. Results: The unequal access to education both before and made worse after climatic events increases the vulnerability of women to climate-related health risks and minimizes their ability to adapt to climate change. Immigrants face increased risk from language barriers, lack of family support, and resource limitations, while the limited access to shelters, stigma and social exclusion increases the vulnerability of homeless populations to climate-induced health conditions. All three focus populations were prone to increased physical and mental health challenges arising from climatic events and are often neglected in climate discourses, planning and response. The provision of temporary and low-cost permanent housing with adequate heating and cooling is recommended to aid in the mitigation and adaptation of these populations to the health effects of climate change. This research underscores the need for more intersectionality studies which factor the multiplicity of identities for effective climate-health equity planning and action. |
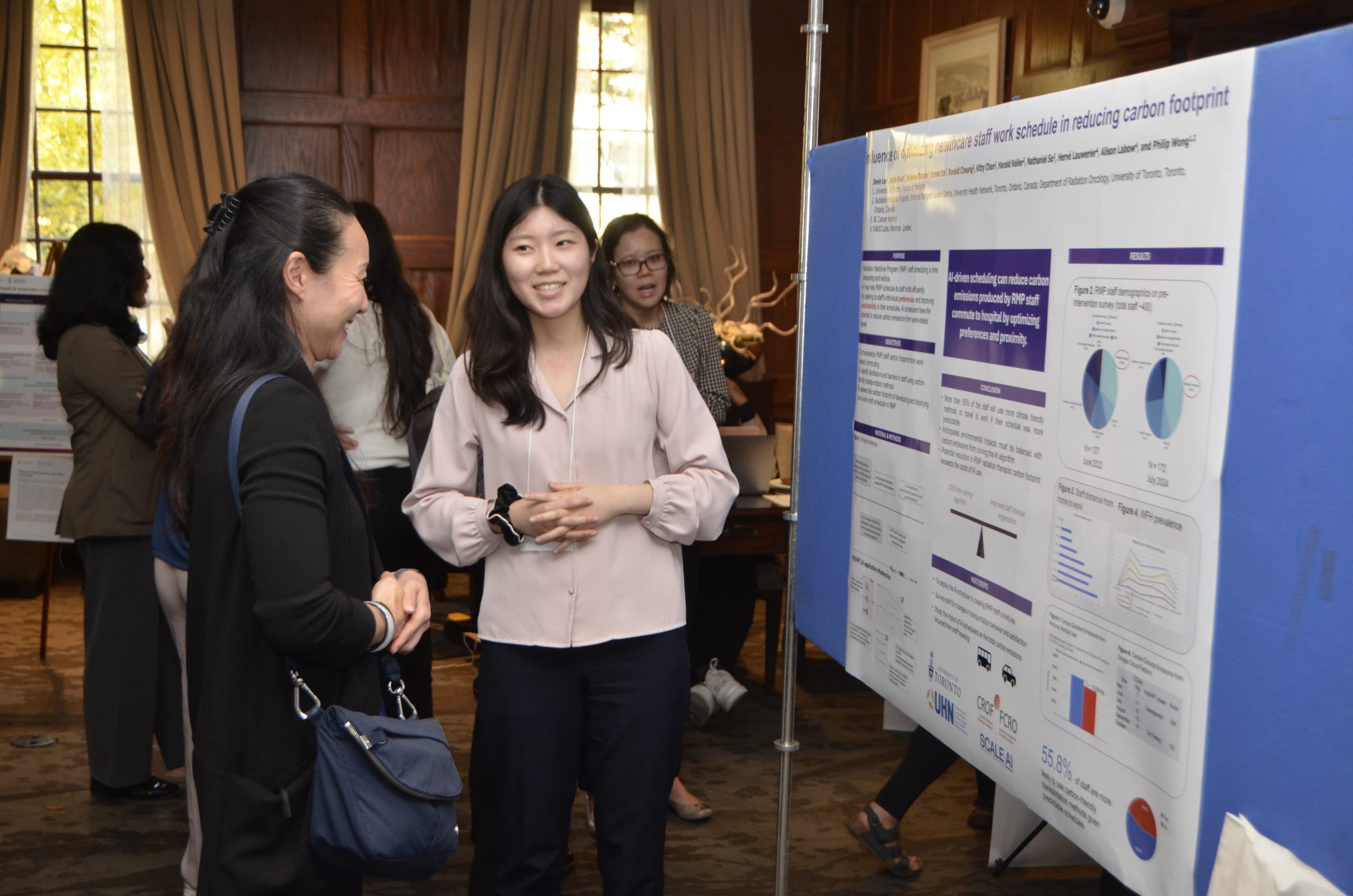
Photos from the event
Please reach out to climate.health@utoronto.ca for more photos from our event!